Update time:2024-04-10Visits:4047
In recent years, gynecological malignancies have been increasingly affecting younger populations, with 15% to 20% of gynecological tumor patients being of childbearing age. As the level of diagnosis and treatment has improved, the cure rate for cancer patients has significantly increased, and more and more patients are hoping to enhance their quality of life and achieve fertility. However, after undergoing treatment, their ovarian function has been impaired to varying degrees, leading to a decline in endocrine function and infertility…

Afflicted with a tumor, they also face the risk of infertility.
In the context of surgery, the target of gynecological malignant tumor operations is the female reproductive organs. While excising the lesions, it is often necessary to partially or even completely remove the corresponding organs, inevitably resulting in damage to reproductive functions.

Furthermore, many patients require additional chemotherapy or radiotherapy. Depending on their type and dosage, chemotherapeutic drugs can have varying degrees of toxic effects on ovarian function. The ovaries are highly sensitive to radiotherapy, and the already limited ovarian follicle pool is often compromised, leading to a further reduction in the number of follicles and premature ovarian failure. Although the uterus is less sensitive to radiotherapy, the muscle layer and blood vessels can still undergo degeneration, affecting uterine volume, muscle elasticity, and endometrial thickness. Consequently, the risks of infertility, miscarriage, and preterm birth are significantly increased.
Can they still become mothers?
Even when afflicted with tumors, many young women still aspire to become mothers. Currently, fertility preservation methods for gynecological cancer patients include fertility-sparing surgeries, ovarian function-preserving drug therapies, and cryopreservation techniques.
Surgical Fertility Preservation

Surgical fertility preservation involves the removal of tumor tissue while retaining the reproductive organs, thereby offering the possibility of future fertility. For conditions such as cervical cancer, endometrial cancer, and ovarian cancer, it is possible to perform tumor resection while preserving fertility, provided that the cases meet the relevant guidelines. Additionally, to prevent damage to ovarian function from radiotherapy, a bilateral ovarian transposition can be performed during surgery to relocate the ovaries outside the radiation field. A case in point is 30-year-old Xiaofei, who was married and childless. She sought medical attention due to bleeding during intercourse for two months and was diagnosed with cervical squamous cell carcinoma. Both she and her family were eager to have a child. Considering that Xiaofei’s lesion was small, there was no lymph node metastasis, and after a rigorous evaluation and discussion, it was determined that she met the criteria for fertility preservation. Professor Hua Keqin’s team performed a fertility-sparing radical trachelectomy for her, removing the affected cervix while preserving the uterine body. Xiaofei was closely followed up postoperatively, and everything was normal. One year later, she was able to conceive naturally. It is crucial to emphasize that fertility-preserving treatment must be based on a strict evaluation, conform to guideline recommendations, and involve meticulous follow-up.
Medication for Ovarian Function Preservation

One of the more commonly reported methods is the use of Gonadotropin-Releasing Hormone Agonists (GnRH-a). Theoretically, pituitary suppression occurs approximately two weeks after the injection of GnRH-a, which inhibits follicular growth and ovulation. Typically, the medication is administered about two weeks before the start of chemotherapy to minimize the damage to follicles caused by chemotherapeutic agents. However, there is ongoing debate and controversy in both domestic and international research regarding the effectiveness of this approach.
Cryopreservation Technology

The third method, which has always piqued everyone’s curiosity, is “cryopreservation.” The subjects of cryopreservation can be embryos, oocytes, or ovarian tissue.
Choosing which method to use is not straightforward and requires a comprehensive consideration of the patient’s specific medical condition, marital status, and fertility desires.
1.Embryo Cryopreservation
After the application of ovulation induction drugs, once the follicles have matured, the eggs are retrieved. These eggs are then fertilized in vitro to form embryos, which are subsequently cryopreserved.
2.Oocyte Cryopreservation
Commonly referred to as “egg freezing,” this process includes the cryopreservation of mature oocytes and the in vitro maturation of immature oocytes followed by their cryopreservation. It is important to note that our country has not yet approved the freezing of eggs for social reasons.
3.Ovarian Tissue Cryopreservation
Several centers abroad have reported successful live births through ovarian tissue cryopreservation followed by autotransplantation. Currently, this method of cryopreservation is the only option available for prepubescent children or patients who urgently need to undergo cancer treatment.
Young patients with gynecological malignancies
Still have the chance to become mothers
However, regardless of the chosen option
Strict screening and comprehensive evaluation are required
Wishing everyone “good luck with pregnancy”
Author Introduction
DZhang Ying
Department of Gynecologic Oncology, Deputy Director of the Party Office, Associate Chief Physician, Master’s Supervisor.
With over ten years of clinical experience in obstetrics and gynecology, Dr. Zhang Ying has accumulated extensive clinical expertise and is proficient in various clinical operative skills in the field. Her specialties include tumor endocrinology and fertility preservation.
Clinic Hours:
Friday mornings and Wednesday afternoons: Fertility Preservation Clinic (Huangpu Campus)
Thursday afternoons: Yangpu Campus
Expert Introduction
Dr. Hua Keqin
Department of Gynecologic Oncology, Party Secretary, Professor, Chief Physician, Doctoral Supervisor.
With over 30 years of clinical experience in obstetrics and gynecology, Professor Hua Keqin has achieved remarkable accomplishments in gynecologic minimally invasive surgery, tumor endocrinology, reproductive tract malformations, and pelvic floor reconstruction, maintaining leading positions both domestically and internationally. She has made innovative contributions, particularly in gynecologic minimally invasive techniques that preserve reproductive organ function.
Clinic Hours:
Tuesday mornings: Yangpu Campus
Wednesday mornings: Huangpu Campus
撰文:邵书铱 张英
审核:王珏
编辑:李妙然
上海市科委科普项目资助(项目编号:20DZ2311000)
Shanghai Medical Pilot Realizes “Walking Dream” for Bulgarian Girl with Cerebral Palsy
A Shanghai Doctor Uses Ultrasound to “Wake Up” Mother's Alzheimer's
Shanghai Medical Trio Stages High-Altitude Rescue on Flight from Xinjiang
Shanghai Children’s Hospital Uses Remote MDT to Diagnose Rare CIPA
Young Girl With Congenital Biliary Atresia Treated in Shanghai
Shanghai Ninth Hospital Saved a Man with Advanced Tongue Cancer
International Medicine at Shanghai Children's Medical Center in 2025
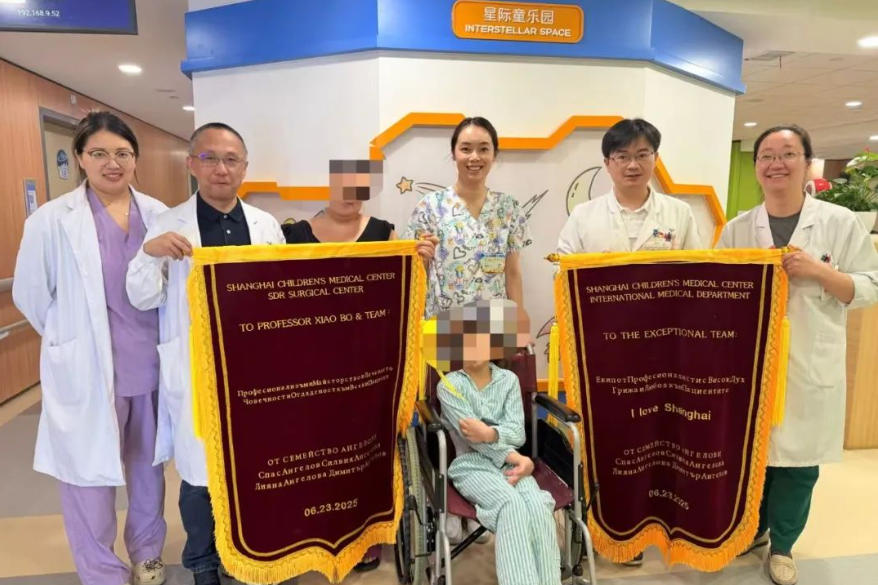
Shanghai Medical Pilot Realizes “Walking Dream” for Bulgarian Girl with Cerebral Palsy
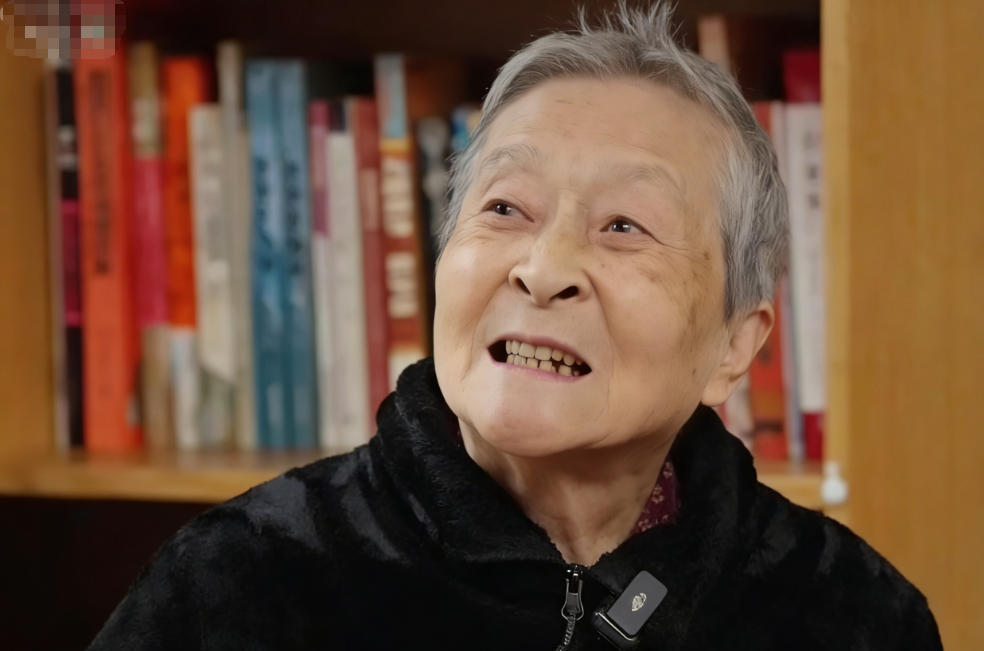
A Shanghai Doctor Uses Ultrasound to “Wake Up” Mother's Alzheimer's

Shanghai Medical Trio Stages High-Altitude Rescue on Flight from Xinjiang

Shanghai Children’s Hospital Uses Remote MDT to Diagnose Rare CIPA

A Seven-Year Lifeline: The Warm Sun of Ovarian Cancer Care

Cosmetic Acupuncture | TCM’s Aesthetic Evolution

Young Girl With Congenital Biliary Atresia Treated in Shanghai

Shanghai Ninth Hospital Saved a Man with Advanced Tongue Cancer

Foreign Tourists Experience TCM in Shanghai

International Medicine at Shanghai Children's Medical Center in 2025